Thrombolysis in Acute Stroke
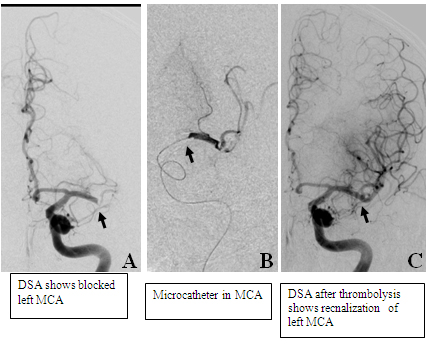
A 64-year-old male presented with suddenonset hemiplegia and aphasia of 4-hours duration. since the time liit for intravenous therapy had already passed, patient was taken up for intra-arterial recnalization. dsa revealed blocked left mca (a). microcthter ws placed in mca and urokinase 95 millio units) was infused resulting in recnalization of mca (c). patient acheived complete clinical recovery.
What is the concept of thrombolysis? What is penumbra zone?
When blood flow to the brain stops, brain cells are deprived of oxygen and nutrients. Stroke is a medical emergency because brain cells start dying quickly and the treatment is most effective when given promptly. Although some of the cells die within few minutes, surrounding zone though hypoperfused but are receiving just enough oxygen from cerebral blood flow (CBF) to stay alive. A compromised cell can survive for several hours in a low-energy state and is referred to as "penumbra". If blood flow is restored within this narrow window of opportunity then some of these cells can be salvaged and become functional again. Blood flow to these cells can be achieved by administrating the clot-dissolving thrombolytic agent t-PA by intravenous and intra-arterial routes.
Who are the right candidates for thrombolysis?
Patients who are able to reach hospital before major infarct has taken place and fulfill the criteria for thrombolysis are the right candidates. Patients with hemorrhage or well-established acute infarct on CT /MRI sequence are not the right candidates. According to the criteria patient's having hypodensity in less than third of MCA territory on CT scan are eligible for thrombolysis.
When is thrombolysis not done?
Thrombolysis is not done in patients who are likely to have hemorrhage with use of thrombolytic drugs. The contraindications include
- CNS lesion with high likelihood of hemorrhage s/p chemical thrombolytic agents (e.g., brain tumors, abscess, vascular malformation, aneurysm, contusion)
- Established Bacterial endocarditis
- There are many relative contraindications including mild or rapidly improving deficits, stroke within 3 months, history of intracranial hemorrhage and major surgery within past 14 days. The complete is always checked beore performing the procedure.
What is likely benefit and risks of thrombolysis?
In the NINDS trial Favorable outcomes were achieved in 31% to 50% of patients treated with rtPA, as compared with 20% to 38% of patients given placebo. The benefit was similar 1 year after stroke. The major risk of treatment was symptomatic brain hemorrhage, which occurred in 6.4% of patients treated with rtPA and 0.6% of patients given placebo. However, the death rate in the 2 treatment groups was similar at 3 months (17% versus 20%) and 1 year (24% versus 28%).In the NINDS trial there was 11-13% absolute increase in the number of people who had minimal or no disability. When tPA was given within 3 hours of onset of symptoms, the number needed to treat for 1 more patient to have a normal or near normal outcome was 8, and the number needed to treat for 1 more patient to have an improved outcome was 3. These NNT are very impressive.
When is intra-arterial thrombolysis done ?
At present intravenous therapy is not recommended beyond 3-hours, although in some cases it may be done upto 4.4 hours. Intra-arterial thrombolysis can work up to 6-hours. Therefore patients coming between 3 to 6 hours can benefit by intra-arterial therapy. The window period can be further extended in cases of posterior circulation stroke. Patients with major vessel blockage such as internal carotid, middle cerebral artery and basilar artery are unlikely to respond to intravenous thrombolysis and can be treated better by intra-arterial means.
What is the role of mechanical means of re-vascularziation in acute stroke ?
One of the disadvantages of using thrombolytic drugs is that there is risk of bleeding. Another issue is that in large vessel blockage thrombolytic drug is not effective. These drugs cannot be used in many situation such as recent surgery. To avoid these problems, mechanical means can be used to takeout the clot and open up the blocked brain blood vessel. One such device is penumbra device in which special catheter can be taken up to the clot which can then be aspirated. Medatna The Medicity is the first center in which such procedure was performed in North India.
What should one do if one sees a patient who is a possible candidate for thrombolysis?
One of the disadvantages of using thrombolytic drugs is that there is risk of bleeding. Another issue is that in large vessel blockage thrombolytic drug is not effective. These drugs cannot be used in many situation such as recent surgery. To avoid these problems, mechanical means can be used to takeout the clot and open up the blocked brain blood vessel. One such device is penumbra device in which special catheter can be taken up to the clot which can then be aspirated. Medatna The Medicity is the first center in which such procedure was performed in North India. One should get a CT scan done immediately to rule out a bleed. If there is no bleed and patient is within the window period then one should transfer the patient immediately to a centre with thrombolysis facilities. No anti-platelet should be given in these patient before thrombolysis. We should add antiplatelet after 24 hrs after excluding hemorrhage by repeat CT scan brain in thrombolysed patients.